You are here
Position Statement 47: Custody Relinquishment and Funding for Care and Treatment of Children
Policy
Mental Health America (MHA) remains resolved that it is inhumane and counter-productive to require families of children with mental health and substance use conditions to relinquish (i.e. give up) parental rights in order to get mental health treatment for their children. Although there are times when the family is part of the problem, there is then work to be done with the family, and effective involvement of the family is often indispensable to a positive and lasting solution in the best interest of the children. Neither foster care nor juvenile justice are good alternatives if there is an option to preserve the family intact.
As of 2002-2004, when the issue of custody relinquishment last received critical federal attention from the General Accounting Office and the Congress, more than 12,700 children were placed into state child welfare or juvenile justice systems each year in order to gain access to mental health care.[1] Some states[2] now outlaw this practice for child welfare,[3] some states and school districts have provided funding to deal with the fundamental problem of lack of resources,[4] and federal law and especially the Affordable Care Act (ACA) now provides an array of benefits to states willing to expand their Medicaid programs.[5]
However, as the Supreme Court’s rejection of the Medicaid mandate[6] has played out in state politics, 22 states (shown in orange below) have not seized these opportunities, with Texas and Florida as the biggest holdouts. This is the January, 2015 map:
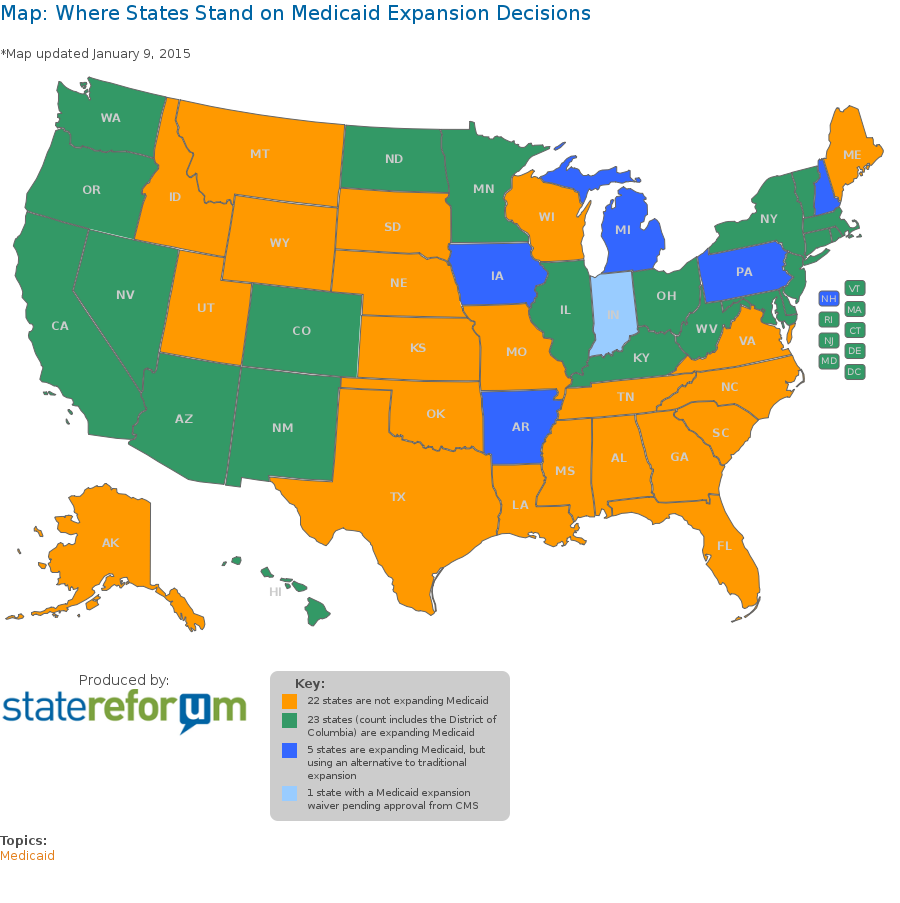
In the orange states, and to some extent in all states where child welfare or juvenile justice treatment is still available as a resource to fill funding gaps, anecdotal information demonstrates that the practice of custody relinquishment continues.[7]
INFORMATION REQUESTED. MHA is interested in documenting the extent of custody relinquishment being required for mental health treatment, and affiliates are encouraged to respond to inappropriate demands for custody relinquishment as a condition for mental health or substance abuse treatment, whenever and wherever they occur. The current data are inadequate to determine how much of a problem remains. Delinquency as well as dependency and neglect proceedings are at issue, since both threats can be used against parents whose advocacy or home atmosphere is perceived as disruptive (as when caring for a sick child) or simply to draw down funding when existing options are exhausted and a child desperately needs treatment.
Background
According to the final report issued by the 2003 President’s New Freedom Commission on Mental Health, the public mental health system as it then existed was “in shambles.”[8] In no place was this more apparent than in the area of children’s services, where lack of crisis services and treatment options have complicated the already fraught issue of when an out-of-home placement is needed for therapeutic or correctional reasons. Barriers to accessing needed mental health treatment often led to parental custody relinquishment to the child welfare or juvenile justice systems. The GAO Report cited in endnote 1 quantified the problem in child welfare but did not address juvenile justice.
Parity. Implementation of federal and state parity laws will help families with access to private health insurance, but not enough. Because benefit plans do not cover a variety of service options, and some states have refused to expand their Medicaid programs, significant financial burdens remain. Some families still must sacrifice savings and retirement accounts and sell personal property as a means to finance the services their child needs to deal with a serious mental health or substance use condition.
EPSDT, IDEA and CHIP. Litigation under the Social Security Act (Medicaid and EPSDT – Early Periodic Screening, Diagnosis and Treatment), IDEA (The Individuals with Disabilities Education Act[9]), and constitutional claims based on the family privacy interests implicated by custody relinquishment have succeeded in developing some resources, especially school-based resources, and CHIP has provided federal funding for health insurance for children, which together have led to a decrease in custody relinquishment cases in the last 10 years.[10] CHIP or CHP programs differ by state: http://www.insurekidsnow.gov/state/index.html
Litigation to require implementation of the ESPDT program[11] and individual appeals under the IDEA have proven very helpful in getting needed services, but IDEA only covers services during the school year, and state disinterest has left many federal promises unfulfilled. The most important of these is Medicaid:
Medicaid Options:
- ACA Medicaid Expansion. At the state’s option, Medicaid eligibility can be expanded to cover all children with family incomes at or below 133% of the federal poverty level (as of 2010, $29,400 for a family of 4, or $14,400 for an individual). Under the ACA, the federal government assumes most of this cost.
- PA separate household approach. Pennsylvania is one of two states[12] that has a Medicaid policy that allows a child to be treated as a separate household, disregarding the financial support provided by the family even though the child remains in the family home, in the custody of the parents. The provision that PA has used is Section 1902 (r)(2) of the Social Security Act that allows states to establish a "less restrictive" income and resource methodology. This has been set forth in PA's Medicaid state plan for more than 15 years. In essence, it allows PA to treat children with disabilities as a separate household. This allows PA to treat disabled children who by themselves would meet the Social Security Income (SSI) disability standards, but could not receive SSI cash payments due to family income and resource limits. Allowing for this less restrictive income methodology has alleviated any need for families to relinquish custody of their children in order for them to qualify for Medicaid.
The PA policy allows families whose family income is high to get coverage for a disabled child under Medicaid. PA had discussions with federal officials several years ago about a premium structure that it wished to apply such families. While PA did not implement the premium structure as planned, additional language was added to the Social Security Act to allow premiums to be charged in such situations. See Social Security Act Section 1902 (a)(10)(A)(ii)(XIII). This issue remains for resolution by PA implementing an equitable fee structure to avoid a windfall to wealthy families.
The services that these children receive include all medically necessary services as required under the OBRA '89 provisions of the Medicaid statute, regardless of whether or not they are included in the state's Medicaid state plan. These children receive a range of services from wraparound to residential placement. Significantly, the State gets standard federal reimbursement for such services. Since the ACA would allow for greater reimbursement for the Medicaid expansion population, this may be a less attractive option than ACA Medicaid expansion for those children who would qualify, but the PA approach has the benefit of being more comprehensive. This is an issue that should be negotiated with HHS; PA’s approach could then be used by other states as a model. - Wrap-Around Care and Other Approaches. Another solution is to provide alternatives to out-of-home placement that also avoid custody relinquishment. For example, CA has a title IV -E waiver under federal child welfare laws for wrap around in-home care as an alternative to out of home placement for kids with serious emotional disturbance. This is not an exhaustive survey, and a total of 484 waivers provide other approaches. http://www.medicaid.gov/medicaid-chip-program-information/by-topics/waivers/waivers_faceted.html MHA welcomes advice from other states, especially as ACA implementation requires restructuring of overlapping waivered programs.
- Demonstration Programs. The 2005 Deficit Reduction Act authorized grants to nine states to take part in the Community Alternatives to Psychiatric Residential Treatment Facilities (PRTF) Demonstration Program. The goal of the program was to provide home and community-based services (HCBS) to children as an alternative to placement in residential treatment facilities, in order to test the health outcomes and cost-effectiveness of these services. An independent evaluation of the state PRTF Demonstration Program, released in May 2012, showed that it succeeded in maintaining or improving children’s functional outcomes in juvenile justice, school functioning, substance abuse, and involvement with child protective services. Further, the treatment costs associated with the demonstrations were on average far lower than institutional alternatives, with an average per capita savings of $20,000 to $40,000. According to the State Policy Advocacy and Reform Center, “many states are now using 1915(c) waivers and considering use of 1915(i) state plan options under the Social Security Act to develop and expand HCBS for this population of children.” https://childwelfaresparc.files.wordpress.com/2013/03/medicaid-and-children-in-foster-care.pdf
- Family Opportunity Act. At the state’s option, certain families of children with disabilities may buy into the Medicaid program. Specifically, Medicaid coverage can be purchased by parents with family incomes of up to 300% of the federal poverty level for children under age 19 whose disabilities meet Supplemental Security Income (SSI) eligibility standards (under the Deficit Reduction Act of 2006). The ACA Medicaid population overlaps this earlier program, but it could be significant that the states that have expanded Medicaid under the ACA could extend Medicaid to families living at 133-300% of poverty by implementing the Family Opportunity Act. As of 2004, about half of the states had implemented a Medicaid buy-in program Enrollment and program data past 2004 are difficult to obtain, and the interaction with the ACA needs to be clarified, but this is a promising avenue to get coverage for people living at up to 300% of poverty for whom ACA premium subsidies are insufficient.[13]
- Coverage until 26. States have the option starting in 2014 to extend Medicaid coverage—including all benefits and EPSDT—to former foster children who have aged out of the system, up to age 26 under the ACA.
A Last Resort. Families that qualify for public assistance must rely on an under-funded public mental health system, which does not consistently provide appropriate access to services or adequate treatment choices. Families that are living in poverty but do not qualify for Medicaid or CHIP are even more desperate. For these reasons, and as a last resort when all else has failed, some families are still faced with accessing mental health care through the child welfare or juvenile justice systems. In order to receive this publicly-funded care, families must relinquish parental custody to the state. This breaking of the parent-child relationship is devastating for the child, family, and community. Even the National Conference of State Legislatures has no updated data on the extent of the custody relinquishment problem that remains. However, its website concedes that between 40 percent and 60 percent of children in foster care have at least one psychiatric disorder and details the state legislation that has been passed to deal with this overarching concern. http://www.ncsl.org/research/human-services/health-oversight-for-children-and-youth-in-foster-care.aspx
Shift to Juvenile Justice. Since the “Great Recession” that began in 2009, the problem has shifted and is now focused on juvenile justice placements rather than child welfare custody relinquishment and foster care placements, but with the same dysfunctional effect:
As cash-starved states slash mental health programs in communities and schools, they are increasingly relying on the juvenile corrections system to handle a generation of young offenders with psychiatric disorders. About two-thirds of the nation's juvenile inmates - who numbered 92,854 in 2006, down from 107,000 in 1999 - have at least one mental illness, according to surveys of youth prisons, and are more in need of therapy than punishment.
"We're seeing more and more mentally ill kids who couldn't find community programs that were intensive enough to treat them," said Joseph Penn, a child psychiatrist at the Texas Youth Commission.[14] “Jails and juvenile justice facilities are the new asylums.”
Juvenile prisons have been the caretaker of last resort for troubled children since the 1980s, but mental health experts say the system is in crisis, facing a soaring number of inmates reliant on multiple psychotropic drugs and a shortage of therapists.
Updating these numbers, Juvenile Offenders and Mental Illness (2014) estimates that 20% of juvenile offenders have severe mental health conditions, 30% have ADHD, and 30% have major depression or bipolar disorder. [15]
Call to Action
Children and families should receive the services required to sustain their mental health without sacrificing their family integrity. Thus, MHA encourages affiliates, families and other concerned individuals and organizations to advocate for more state laws banning custody relinquishment requirements and for increased availability, accessibility, and appropriateness of mental health and substance abuse treatment. The federal government has passed laws to help states to shoulder this burden. It is now for the mental health movement to convince the states to respond rationally and compassionately to the opportunity we now have to end custody relinquishment and keep families intact through mental health crises.
Parents should be provided with full information about the mental health and substance use treatment services that are available to address the needs of their child. Community-based services designed to eliminate the need for custody relinquishment should be created, implemented and sustained. This is the only way to further positive outcomes and family preservation. MHA urges the following advocacy agenda:
- Every state should follow the intent of the ACA and expand its Medicaid and CHIP programs to the limits provided by federal law.
- States should consider the PA, MA or CO separate household models for those disabled children who don’t qualify under ACA Medicaid expansion.
- The Family Opportunity Act and other Medicaid buy-in mechanisms should be fully explored to maximize federal help up to 300% of poverty, by careful coordination with ACA subsidies to maximize coverage for people unable to afford it under the ACA.
- Insurance parity should be enforced to provide equal mental health coverage and the increased service options that children with mental health and substance use conditions need to ensure their health and wellness.
- The provisions of the Social Security Act (Medicaid and EPSDT), IDEA, and constitutional claims based on the family privacy interests implicated by custody relinquishment should be actively litigated to fight loss of custody and increase treatment options.[16]
- In addition to maximizing federal and insurance funds, states facing a funding gap like TX and CO should explore options like those enacted by both of those states to appropriate state funds to avoid custody relinquishment and assure needed treatment services and care management.
Effective Period
The Mental Health America Board of Directors approved this policy on March 7, 2015. It will remain in effect for five (5) years and is reviewed as required by the Public Policy Committee.
Expiration: December 31, 2020
[1] CHILD WELFARE AND JUVENILE JUSTICE: Federal Agencies Could Play a Stronger Role in Helping States Reduce the Number of Children Placed Solely to Obtain Mental Health Services (GAO-13-397, April 21, 2003). http://www.gao.gov/new.items/d03397.pdf. Estimate based on national survey conducted in 2001. See, generally, “Staying Together: Preventing Custody Relinquishment for Children’s Access to Mental Health Services,” Bazelon Center for Mental Health Law and Federation of Families for Children’s Mental Health (1999) and “Relinquishing Custody: The Tragic Result of Failure to Meet Children’s Mental Health Needs,” Bazelon Center for Mental Health Law (2000), both available from Bazelon. PDF version of 1999 publication available at http://www.bazelon.org/issues/children/publications/stayingtogether/staying2.pdf.
[2] As of 2003, eleven states permitted access to child welfare services without loss of custody, and six states plus the District of Columbia forbade voluntary provision of child welfare services altogether. The remaining states had no clear policy on custody relinquishment. Id. This list has not been updated by the GAO or Bazelon nor is more recent information available from the National Conference of State Legislatures. Many states have acted since then, but state performance depends on the appropriations process as well as substantive law, so the extent of the problem is difficult to quantify. A 2010 Colorado statute takes the bold step of creating a state-funded safety net for children’s mental health services, using the separate household approach:
Colo. Rev. Stat. 27-67-104. Provision of mental health treatment services for youth
(1) (a) A parent or guardian may apply to a mental health agency on behalf of his or her minor child for mental health treatment services for the child pursuant to this section, whether the child is categorically eligible for medicaid under the capitated mental health system described in section 25.5-5-411, C.R.S., or whether the parent believes his or her child is a child at risk of out-of-home placement. In such circumstances, it shall be the responsibility of the mental health agency to evaluate the child and to clinically assess the child's need for mental health services and, when warranted, to provide treatment services as necessary and in the best interests of the child and the child's family. Subject to available state appropriations, the mental health agency shall be responsible for the provision of the treatment services and care management, including any in-home family mental health treatment, other family preservation services, residential treatment, or any post-residential follow-up services that may be appropriate for the child's or family's needs. For the purposes of this section, the term "care management" includes, but is not limited to, consideration of the continuity of care and array of services necessary for appropriately treating the child and the decision-making authority regarding a child's placement in and discharge from mental health services. A dependency or neglect action pursuant to article 3 of title 19, C.R.S., shall not be required in order to allow a family access to residential mental health treatment services for a child.
[3] A 2006 Virginia Attorney General’s opinion ruled that §2.-5211(B)(3) of the Virginia Comprehensive Services Act (CSA) requires the state and localities to serve children who are at risk of foster care placement without requiring their parents to relinquish custody. In Missouri, under SB 1003 (2004), Section 630.097, RSMo established a comprehensive children's mental health service system to serve children in the least restrictive environment. http://www.senate.mo.gov/04info/billtext/tat/sb1003.htm This legislation has effectively ended custody relinquishment in MO.
[4] In Colorado, a one million dollar state general fund subsidy is still required, despite full Medicaid expansion and a robust CHIP program. In contrast, in California, the 2005 Proposition 63 ballot measure included language providing that if access to mental health care was the cause of relinquishment and there was no other funding source to pay for it, counties could provide Prop 63 funds to a family to pay for the care. This has been in the law for 10 years, but no one has used it, in part because CA also has a title IV -E waiver under federal child welfare laws for wrap around in-home care as an alternative to out of home placement for kids with serious emotional disturbance. But this is a bad solution since technically the family has given up custody in those cases even though the child remains at home. This is a very widely used approach.
[5] States need to develop their children’s mental health service system with funding that allows for flexibility beyond the constraints of Medicaid rather than disrupting families to fit into the constraints of a particular funding stream. This should include state funds to cover non-Medicaid-eligible children and maximizing funding from available commercial insurance coverage, then supplementing it with state funds to fill the gap. Often, public mental health programs are not designed in a way to accept private insurance payment or even to accept private payment from the family. This is because the entire public community mental health system has been designed with the goal of obtaining maximum Medicaid funding.
[6] See Nat’l Fed’n of Indep. Bus. v. Sebelius (NFIB), 132 S. U.S. 2566 (2012), http://www.law.cornell.edu/supremecourt/text/11-393
[7] Texas, the only state for which coded data was obtained, documented that in 2008, in three of 788 cases of child welfare funding based on “refusal to assume parental responsibility,” the underlying reason was “lack of mental health services.” As of 2014, despite an array of state initiatives to decrease reliance on custody relinquishment, Texas estimated an ongoing gap of 60 RTC beds as well as a need for more wrap-around and prevention services: “The collaborative DFPS/DSHS RTC Project has been successfully diverting parents/guardians from relinquishing custody of their children with SED to DFPS by placing children who meet RTC criteria in DSHS-funded RTC beds. However, the 20 children on the RTC waiting list at the end of September 2014 exceed the current capacity of the RTC Project, which is funded for 10 ongoing beds in fiscal year 2014-2015. To date, the project reportedly has effectively prevented the relinquishment of 61 children since the project officially launched with the first RTC placement in January 2014. It is recommended that the number of available RTC beds be increased by 20, for a total of 30 ongoing RTC beds per year. With an expected average length of stay of 6 months, about 60 children would be served per year and diverted from DFPS conservatorship.” Department of Family and Protective Services and Department of State Health Services Joint Report on Senate Bill 44 (December 2014).
[8] http://store.samhsa.gov/product/Achieving-the-Promise-Transforming-Mental-Health-Care-in-America-Executive-Summary/SMA03-3831
[9] P.L. 108-446 (December 3, 2004), 20 USC§1400.
[10] This information is purely anecdotal. The last known survey was the GAO survey, conducted in 2001.
[11] “Medicaid EPSDT Litigation,” produced by Jane Perkins, National Health Law Program (October 2, 2009), http://www.acmhai.org/pdf/jane_perkins_-_epsdt_litigation.pdf
[12] The other is Massachusetts.
[13] Health and Disability Advocates strongly advocates post-ACA continuation of Medicaid buy-in programs. “why Medicaid Buy-in Programs Must Continue After 2014, nchsd.org/library/file.asp?id=300896:
“In general, Medicaid Buy-In programs are accessed by two groups, which are not mutually exclusive:
The first group, usually individuals with a serious mental illness or another chronic condition such as Multiple Sclerosis or AIDS, use MBI programs as secondary, or wraparound, coverage to their primary insurance, Medicare. Without the Medicaid Buy-In, these individuals would lose access to this secondary coverage for Medicare. The costs of their drug coverage and other medical services would rise. They would be forced to quit their jobs in order to maintain affordable and comprehensive Medicaid coverage for their medical conditions.
The second group uses a MBI program to access services not covered by Medicare or any type of private insurance, such as long term care services and state Medicaid waiver services, including services such as personal attendant care. These services are critical to individuals with conditions that limit their daily activities, and they will need to access them through Medicaid, with or without a Buy-In program. Medicaid Buy-In programs simply allow these individuals to work and increase their financial independence while keeping these critical medical services. Take away the Medicaid Buy-In program and Medicaid will still have to provide the services, it is just that the individuals will have to quit their jobs in order to meet the lower income limits for other Medicaid programs.
None of the new options created under the ACA will provide these individuals with the comprehensive coverage necessary for their conditions. Newly-eligible Medicaid is not available to most of them because they are Medicare beneficiaries. For those who are not, there is no guarantee that the new category of Medicaid will cover the long term care services that they may need. Private insurance policies sold through the newly developed State Insurance Exchanges will likely be unavailable or inadequate for most of them for the same reasons.”
[14] Acting Director of the Texas Youth Commission which provides mental health services to the state's juvenile correctional system.
[15] New York Times, “Mentally Ill Offenders Strain Juvenile [Justice] System,” by Soloman Moore, August 10, 2009; Marvin D Feit, John S Wodarski, Catherine Dulmus, and Lisa A. Rapp-Paglicci, Juvenile Offenders and Mental Illness: I Know Why the Caged Bird Cries (Routledge 2014).
[16] Bazelon: Litigation Strategies (out of date): http://www.bazelon.org/issues/children/custody/litigation.htm







this page